Fact Checked
This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
August 6, 2018
Experts consider tenesmus to be both a physical and mental condition. It feels as if there is stool to pass, but there usually isn’t. Tenesmus is different than diarrhea because when you go to the bathroom not much, or nothing at all comes out. The sensation of needing to poop can be caused by faulty nerve signals or small amounts of stool stuck in the rectum due to constipation.
Many people describe tenesmus as a very distressing symptom because you never know when it’s going to be triggered and return.
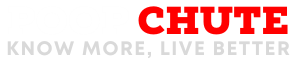
How long does tenesmus last? It depends on the underlying cause. Symptoms can last for weeks or months. Women are more frequently affected by tenesmus than men, since they experience more GI issues in general. Some people experience chronic tenesmus that comes and goes. Tenesmus can be temporary if it’s caused by an infection, acute traumatic stress, surgery or another short-term illness. If IBS, IBD or cancer is causing tenesmus, then it’s likely that it will return from time to time without treatment.
Treating tenesmus usually involves identifying the underlying cause (such as inflammatory bowel disease, IBS or an infection), making lifestyle and diet changes, and sometimes taking medications to control symptoms if needed.
What Is Tenesmus?
Tenesmus is defined as “the sensation of urgently needing to evacuate the bowels even though they are empty.” (1) It’s one of the most common symptoms associated with inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis. (2) Tenesmus is sometimes called rectal tenesmus because it primarily results from inflammation of the rectum, the final section of the large intestine that ends at the anus.
Vesical tenesmus is similar to rectal tenesmus, but instead of affecting the rectum it affects the bladder. Vesical tenesmus is characterized by the feelings of being unable to completely empty the bladder and having to frequently urinate even though not much urine comes out.
Tenesmus Symptoms & Signs
The most common tenesmus symptoms include: (3)
- Feeling like you need to go to the bathroom (empty the bowels) right away. This can happen suddenly out of nowhere, or right after you finish using the bathroom. You might get up from the toilet and feel like you need to sit right back down again, but then nothing will actually happen.
- Having multiple very small bowel movements throughout the day.
- Abdominal pain and discomfort. Pain usually goes away after passing a bowel movement.
- Cramping in the intestines and stomach.
- Straining when trying to go to the bathroom.
- Feeling like you cannot completely empty the bowels. This can be associated with constipation, which may come while you’re dealing with tenesmus.
- Anxiety and distress over dealing with tenesmus, including reduced quality of life, trouble sleeping, insecurity around others, and nervousness about when the symptoms will return.
- Depending on the cause of your tenesmus, you might also experience signs of an infection, such as a fever. If tenesmus is caused by cancer affecting the colon/rectum, then it’s also possible to have blood in your stools.
Tenesmus Causes & Risk Factors
The most common reason that people experience tenesmus is due to inflammatory bowel disease (IBD), or Crohn’s disease and ulcerative colitis. It’s believed that tenesmus affects people with ulcerative colitis (UC) more often than those with Crohn’s disease because of how UC causes rectal hypersensitivity, although both conditions can cause tenesmus.
Aside from IBD, other tenesmus causes can include:
- Irritable bowel syndrome (IBS).
- Anxiety.
- A colonoscopy or surgery that affects the bowels.
- Infections that affect the gut/digestive system, which rarely can include sexually transmitted diseases like chlamydia, that may lead to pelvic inflammation. (4)
- Motility disorders that affect movement of the intestines.
- Pregnancy and sometimes PMS or PMDD.
- Radiation of the rectum or colon (called radiation proctitis or colitis).
- Anorectal abscess, a painful condition that causes pus to develop near the anus.
- Colon cancer, colorectal cancer or tumors.
What exactly causes the constant urge to poop? The underlying reason that tenesmus occurs is due to inflammation of the bowel. The bowel is considered the part of the alimentary canal in the digestive system that is located below the stomach, including the small intestine, large intestine/colon and rectum.
Dysfunction of the rectum usually seems to be involved in development of tenesmus. The small nerves and muscles in the rectum can start to cramp and spasm, leading to the urgent sensation of needing to use the bathroom. Some patients are told they have “rectal hypersensitivity,” especially those with IBS, which a term that describes faulty signals being sent between the bowels and brain. One study found that 64 percent of IBS patients experienced rectal hypersensitivity, especially “alternating IBS patients” (constipation and diarrhea) but less commonly those with constipation-predominant IBS. (5)
Can stress cause tenesmus? Severe stress may trigger tenesmus in people who are susceptible to digestive issues, such as those with IBD or IBS. However, normal amounts of everyday stress alone should not cause tenesmus. The reason stress impacts digestion so much is because the gut is closely connected to the brain. The two actually communicate constantly via a large nerve called the vagus nerve, which sends signals from your central nervous system (brain and spine) to your gastrointestinal (GI) system (6). In response to stress, your GI system is capable of producing, or not producing, certain neurotransmitters, such as serotonin, which have important implications for how you feel.
Risk factors for developing tenesmus include:
- Untreated food sensitivities and allergies (especially to things like dairy, gluten and other FODMAP foods, which contain certain carbohydrates).
- Eating a poor diet that can increase inflammation.
- Chronic stress or temporary high amounts of emotional or physical stress.
- Having a family history of IBD or IBS.
- Sedentary lifestyle with little or no exercise.
- Low immune function, which can increase risk for infections.
- Personal or family history of colon or rectal cancer. Smoking, drug use and alcoholism can all increase the risk for these cancers.
- Older age, which can cause a range of digestive issues.
- Use of certain medications that interfere with digestive health.
- History of untreated sexually transmitted diseases.
- Other sources of stress like traveling, illness, and lack of sleep.
- Changes in sleep routine and circadian rhythm.
- Hormonal imbalances or changes (menstruation, menopause or pregnancy might bring on symptoms).
Conventional Treatments for Tenesmus
If you visit your doctor for help with resolving tenemus, he or she will most likely ask about your symptoms, history of gastrointestinal disorders, and perform a rectal exam. Other tests might also be needed to identify the underlying cause of tenesmus. These tests can include: colonoscopy to look at the colon and rectum, blood test, CT scan and stool culture test.
What type of tenesmus treatment medications are available?
- Anti-inflammatory agents and/or immunomodulators.
- Antispasmodics, which are smooth muscle relaxers.
- Tricyclic antidepressants (TCAs) are sometimes used to manage tenesmus symptoms associated with stress, anxiety or IBS. Other selective serotonin reuptake inhibitors (SSRIs) and agents that modulate chloride channels and serotonin are also prescribed. Unfortunately, these drugs commonly cause side effects, which can potentially include dry mouth, dry eyes, weight gain, sedation, urinary retention and visual changes.
- Anticholinergics, which are usually taken before meals if this is when symptoms usually start.
- Anticonvulsants, which are used to treat chronic pain.
- Use of antibiotics and probiotics (“good bacteria” that colonize the gut) if an infection is present.
- If tenesmus causes pain and cramping, your doctor might recommend you take ibuprofen or another over-the-counter pain killer.
- Pain killers, including strong medications like methadone, which can be used to treat tenesmus in some cases. These tend be a last report option in patients with advanced stage cancer who are experiencing ongoing pain that doesn’t resolve with other treatment. (7)
- Rarely, endoscopic and surgical therapy is needed.
It can be difficult to treat tenesmus in patients with advanced cancer, which is very distressing. Surgery, radiotherapy and/or chemotherapy do not usually help resolve tenesmus and might even make it worse. (8) Cancer patients with tenesmus can sometimes find some relief by taking the medications above, improving their diet and treating constipation or diarrhea.
6 Natural Treatments for Tenesmus
1. IBD/IBS Diet Plan
The journal Clinical Advances in Gastroenterology states that in patients with IBS or IBD “Abdominal pain, bloating, constipation and diarrhea are the four main symptoms that can be addressed using a combination of dietary interventions and medications.” (9) One of the first steps to take if you have tenemus is to address your diet. Eating a whole foods, nutrient-dense diet is key for reducing underlying inflammation in the bowels.
- Aim to eat a healing diet that consists of eating roughly equal amounts (33 percent each) of clean protein sources, healthy fats, and low-glycemic carbohydrates in the forms of tolerable fruits and vegetables.
- Eat probiotic foods, like cultured veggies (sauerkraut or kimchi), and fermented yogurt or kefir if they are tolerated well. If they don’t worsen symptoms, also have prebiotic foods including asparagus, bananas, honey, garlic and oats,
- Add enough healthy fats to your diet, like coconut oil, olive oil, butter, ghee and avocado. Avoid having lots of fat at one time, which can sometimes worsen symptoms.
- Drink bone broth daily, or use protein powder made from bone broth, which can be healing to the gut.
- Fresh herbs and spices should be added to meals, including rosemary, fennel, ginger, mint, basil and turmeric.
- Avoid processed grains, especially those containing wheat/gluten. Also consider trying a low fructose diet, since high amounts of fructose (sugar) can contribute to symptoms. Foods to limit or avoid include: added white sugar, chocolate, high fructose corn syrup, processed corn and potato products, honey, wheat products (cereals, bread, cakes, cookies), soda, fruit juices, artificial sweeteners and high fructose fruits like apples, watermelon, pears and grapes.
- Avoid dairy products until you are certain that lactose intolerance is not playing a role in your symptoms.
- Try an elimination diet in which you give up common allergens (including eggs, nuts, shellfish), spicy foods and certain FODMAP grains, veggies and fruit (such as apples, stone fruit, avocado, onions, garlic and broccoli) to test your reaction.
- Eating smaller meals will put less stress on the gastrointestinal tract, which can help reduce some symptoms.
2. Natural Diarrhea Remedies
If you experience on-and-off again diarrhea and tenesmus at the same time, there are certain things you can do to help treat diarrhea naturally.
- Prevent dehydration by drinking water throughout the day.
- Eat bananas and rice, which can help to “bind” loose stools.
- Add raw honey and ginger root to tea to soothe your stomach.
- Try having flaxseed oil, which has been shown to reduce the duration of diarrhea.
- Avoid having caffeine and alcohol (or at least limit the amount).
- Avoide eating too much unripe or overripe fruit.
- Limit greasy food that is difficult to digest properly.
- Manage stress and get enough rest.
- Skip tough/intense workouts until you are feeling better.
- Talk to your doctor if you take medications that cause diarrhea such as antacids, antibiotics, quinidine, lactulose and colchicine.
3. Natural Constipation Remedies
Constipation and tenesmus commonly occur together because being constipated makes you feel like you haven’t fully emptied your bowels and need to try again. Constipation can also lead to straining and cramping, two symptoms that usually occur with tenesmus.
There are a number of natural laxatives that can also help prevent and treat constipation. Tenesmus home remedies that can help break the constipation-tenesmus cycle include:
- High fiber foods, which can help to add bulk to the stool, making it easier to have regular bowel movements. These include: cooked veggies, fruits (including prunes or figs), seeds like flax or chia, nuts, and cooked starchy veggies. However, keep in mind that in people with IBS who often have diarrhea and symptoms of bloating, fiber may make symptoms worse. For these people, reducing fiber intake may improve symptoms, so it can take some trial and error to find the right amount of fiber that works best for you.
- Drink plenty of water, which helps fiber do its job. You can also add apple cider vinegar or fresh lemon juice to water, which can be stimulating. Fresh vegetable juices and coconut water are other hydrating drinks that may help with digestion.
- Use peppermint oil, whether topically or taken internally with water. This has a soothing effect on the stomach and often helps with IBS symptoms.
- Try magnesium supplements or magnesium oil, which helps to prevent muscle spasms and also lubricates stools so they are easier to pass.
- Drink aloe vera juice (half cup three times daily), which helps naturally reduce constipation by acting as a lubricant.
- Eat smaller, balanced meals throughout the day, rather than two to three large meals. Try to keep meal times consistent to help get your body more regular.
- Herbs including slippery elm, licorice root and ginger can all help soothe intestinal inflammation and indigestion.
If you have hemorrhoids or bloody stools, cleanse yourself only with natural soaps that don’t contain harsh chemicals, alcohol or perfumes. Use plain water to wipe yourself and then dry your bottom afterward. You may also want to try making a homemade Hemorrhoid Cream with Turmeric & Tea Tree Oil to soothe irritation.
4. Managing Stress
- Try meditating, prayer, yoga, deep breathing exercises, and keeping a journal to track your feelings.
- See a therapist or counselor if you’re dealing with chronic stress or trauma.
- Spend more time outdoors each day and get exposure to natural sunlight.
- Find a support group, spiritual center or another group to join that helps you feel more connected to others.
- Get enough sleep every day, ideally around seven to nine hours. Sleep in a dark, cool room that is comfortable and free from distractions. Try to go to sleep and wake at roughly the same each day, which helps regulate your body’s “internal clock.”
- Use relaxing essential oils to help lower stress while also fighting inflammation, including ginger, peppermint, lavender and fennel essential oil.
- Another important step for reducing physical oxidative stress is quitting smoking, limiting alcohol consumption, and limiting caffeine/stimulant use.
5. Exercise
Exercise is a natural way to reduce inflammation and also helps to get the bowels moving. A 2011 study published in the American Journal of Gastroenterology found that increased physical activity improves GI symptoms associated with IBS and improves quality of life. (10) Physical activity has been shown to be effective in the treatment of depression, anxiety and stress-related conditions. Try to be active for at least 30–60 minutes per day. Exercising in the morning can be helpful for regulating bowel movements, and it’s a bonus if you can exercise outside, which also allows you to get some vitamin D.
6. Supplements
Besides those mentioned above, supplements that can help prevent IBS/IBD symptoms include: (11)
- Probiotics (50 billion to 100 billion units daily) — Probiotics help recolonize the gut with healthy bacteria.
- Digestive enzymes (two before each meal) — These can help with indigestion by regulating stomach acid and nutrient absorption.
- Omega-3 fish oil (1,000 milligrams daily) — Helps to reduce inflammation in the GI tract.
- Adaptogen herbs — Help lower the effects of stress and hormonal imbalances.
- L-glutamine powder (5 grams twice daily) — Helps repair the digestive tract, especially important for people with chronic diarrhea or leaky gut syndrome.
Precautions Regarding Tenesmus
If your tenesmus symptoms are severe enough to interfere with your quality of life, if they keep returning and if they don’t respond to treatment, then talk to your doctor right away to rule out serious underlying health conditions. If you develop any of the following symptoms, talk a medical professional right away to prevent symptoms from getting worse:
- Bloody stools.
- Intense abdominal pain.
- Signs of infection like fever, chills and body aches.
- Persistent nausea and vomiting, which may lead to dehydration and electrolyte imbalance.
- Ongoing loss of appetite and weight loss.
Key Points about Tenesmus
- Tenesmus is the sensation of urgently needing to evacuate the bowels even though they are already empty.
- Symptoms of tenesmus include cramping, frequent small bowel movements, constipation, pain, diarrhea and sometimes signs of an infection or illness like a fever and bloody stools.
- Underlying tenesmus causes can include: inflammatory bowel disease, IBS, infections, hormonal changes, stress, or colon/rectal cancer.
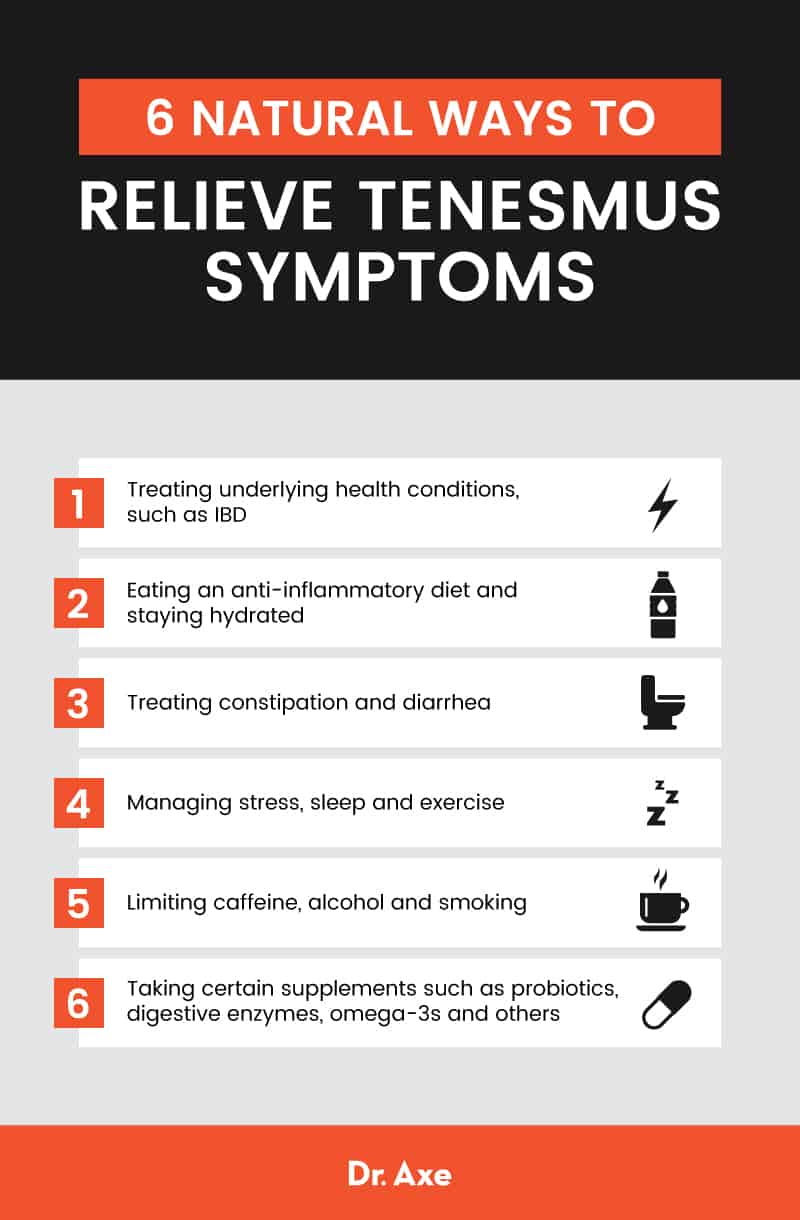
6 Natural Ways to Relieve Tenesmus Symptoms
- Treating underlying health conditions, such as IBD
- Eating an anti-inflammatory diet and staying hydrated
- Treating constipation and diarrhea
- Managing stress, sleep and exercise
- Limiting caffeine, alcohol and smoking
- Taking certain supplements such as probiotics, digestive enzymes, omega-3s and others