The tutorial content material on this submit, elaborated in collaboration with Bromatech, was independently developed and accredited by the GMFH publishing crew and editorial board.
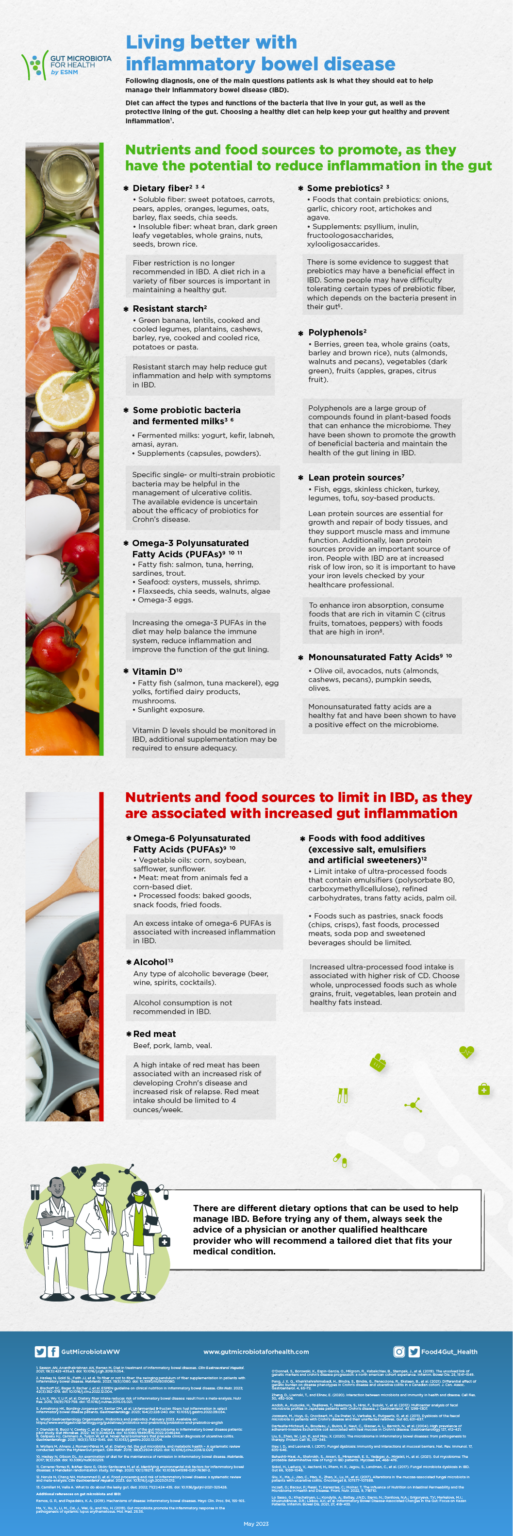
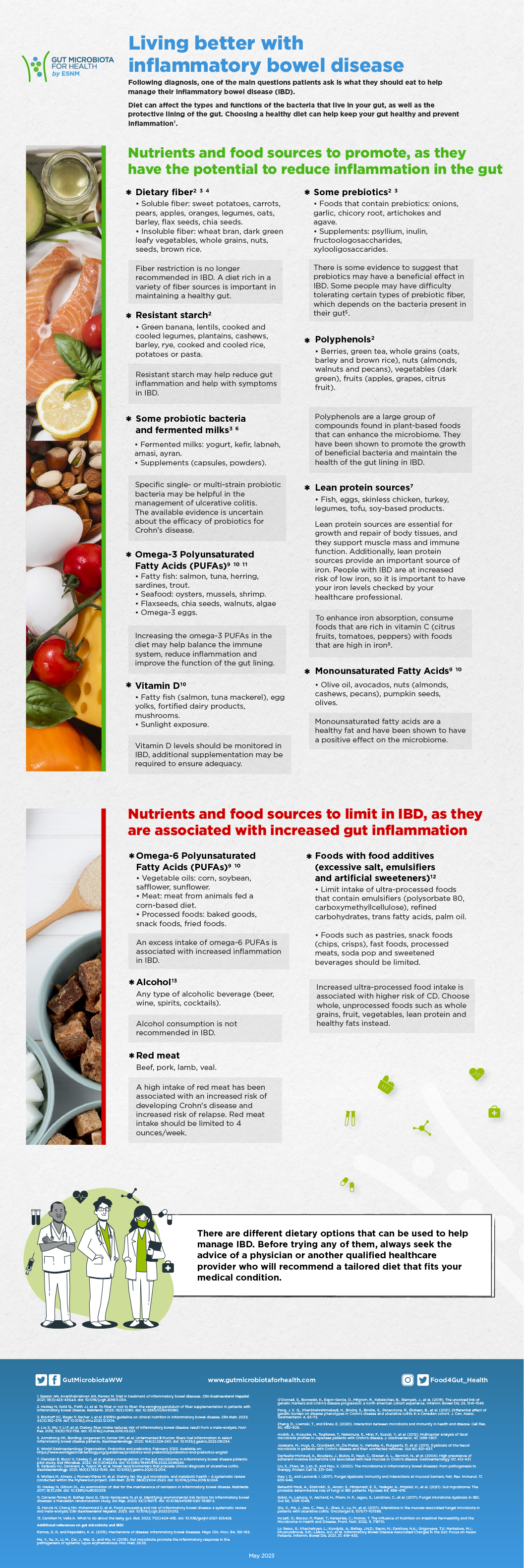
What you eat issues for managing ulcerative colitis and Crohn’s illness. Food regimen can have an effect on the kinds and capabilities of the intestine microbiota, in addition to the intestine’s protecting lining. Though there is no such thing as a particular meals or food plan that may stop or treatment ulcerative colitis and Crohn’s illness, food plan might help preserve your intestine wholesome and stop irritation.
Probably the most broadly studied food plan remedy for IBD is an all-liquid, formula-based meal-replacement food plan (known as unique enteral diet or EEN). EEN supplies all of the important vitamins from the system, whereas excluding all different meals. EEN has been proven to have a number of advantages, together with inducing remission (youngsters), lowering irritation, selling mucosal therapeutic and enhancing dietary standing. Finally, EEN is for use for an outlined time period, then meals is progressively re-introduced.
Whereas there is no such thing as a good food plan that works for everybody with IBD, Natasha Haskey, PhD, who’s a skilled registered dietitian with a give attention to IBD, defined to GMFH editors through electronic mail {that a} Mediterranean-like food plan is advisable for people with IBD trying to eat a extra wholesome balanced food plan and cut back irritation.
Excessive ranges of consumption of greens, fruit, nuts, legumes, olive oil and lean protein sources have been proven to have a protecting impact in opposition to growing IBD in addition to contribute to a wholesome intestine microbiota. In distinction, Western dietary patterns, excessive in omega-6 polyunsaturated fatty acids, alcohol, purple meat and meals components (extreme salt, emulsifiers and synthetic sweeteners) promote intestinal irritation and may worsen signs, and thus ought to be restricted.
Fat are an vital nutrient to concentrate to in IBD. Natasha’s PhD analysis centered on learning the impression of dietary fat in a rodent mannequin with continual colitis. Based on Natasha: “We noticed {that a} food plan wealthy in omega-6 polyunsaturated fatty acids (generally present in corn, soybean, safflower and sunflower oils) promoted irritation. In distinction, a food plan that was wealthy in olive oil and contained omega-3 polyunsaturated fatty acids (from fish) and a few saturated fats (milk fats) promoted immune homeostasis in ulcerative colitis.” Primarily based on these findings, in IBD it might be prudent to scale back the content material of omega-6 polyunsaturated fatty acids within the food plan and enhance the omega-3 polyunsaturated fatty acids and olive oil together with a food plan wealthy in fruit, greens, complete grains with some dairy consumption.
As for when food plan might help probably the most, Haskey acknowledges that food plan might help handle signs and irritation in each lively illness and remission. Nonetheless, given that every affected person has their very own microbial and genetic make-up, probably the most acceptable food plan ought to be personalised. Based on Natasha: “The food plan must be personalised to every particular person, contemplating their illness and what works inside their way of life. Consulting with a dietitian with experience in managing IBD is important to develop an individualized plan.”
As our data concerning the impression of food plan on managing IBD improves, there are extra alternatives to make use of food plan as a supplementary remedy to manage irritation and alleviate signs. Earlier than selecting one of many fad diets promoted for IBD on-line, communicate to your healthcare supplier to allow them to advocate a customized consuming plan that works for you.
In the meantime, this infographic is an efficient start line for contemplating the dietary parts that ought to be promoted and restricted for residing higher with IBD:
References used on the infographcic:
- Sasson AN, Ananthakrishnan AN, Raman M. Food regimen in remedy of inflammatory bowel illnesses. Clin Gastroenterol Hepatol. 2021; 19(3):425-435.e3. doi: 10.1016/j.cgh.2019.11.054.
- Haskey N, Gold SL, Religion JJ, et al. To fiber or to not fiber: the swinging pendulum of fiber supplementation in sufferers with inflammatory bowel illness. Vitamins. 2023; 15(5):1080. doi: 10.3390/nu15051080.
- Bischoff SC, Bager P, Escher J, et al. ESPEN guideline on scientific diet in inflammatory bowel illness. Clin Nutr. 2023; 42(3):352-379. doi: 10.1016/j.clnu.2022.12.004.
- Liu X, Wu Y, Li F, et al. Dietary fiber consumption reduces threat of inflammatory bowel illness: end result from a meta-analysis. Nutr Res. 2015; 35(9):753-758. doi: 10.1016/j.nutres.2015.05.021.
- Armstrong HK, Bording-Jorgensen M, Santer DM, et al. Unfermented b-fructan fibers gas irritation in choose inflammatory bowel illness sufferers. Gastroenterology. 2023; 164(2):228-240. doi: 10.1053/j.gastro.2022.09.034.
- World Gastroenterology Organisation. Probiotics and prebiotics. February 2023. Obtainable on: https://www.worldgastroenterology.org/pointers/probiotics-and-prebiotics/probiotics-and-prebiotics-english
- Olendzki B, Bucci V, Cawley C, et al. Dietary manipulation of the intestine microbiome in inflammatory bowel illness sufferers: pilot research. Intestine Microbes. 2022; 14(1):2046244. doi: 10.1080/19490976.2022.2046244.
- Galipeau HJ, Caminero A, Turpin W, et al. Novel fecal biomarkers that precede scientific prognosis of ulcerative colitis. Gastroenterology. 2021; 160(5):1532-1545. doi: 10.1053/j.gastro.2020.12.004.
- Wolters M, Ahrens J, Romaní-Pérez M, et al. Dietary fats, the intestine microbiota, and metabolic well being – A scientific assessment carried out inside the MyNewGut mission. Clin Nutr. 2019; 38(6):2504-2520. doi: 10.1016/j.clnu.2018.12.024.
- Haskey N, Gibson DL. An examination of food plan for the upkeep of remission in inflammatory bowel illness. Vitamins. 2017; 9(3):259. doi: 10.3390/nu9030259.
- Carreras-Torres R, Ibáñez-Sanz G, Obón-Santacana M, et al. Figuring out environmental threat elements for inflammatory bowel illnesses: a Mendelian randomization research. Sci Rep. 2020; 10(1):19273. doi: 10.1038/s41598-020-76361-2.
- Narula N, Chang NH, Mohammad D, et al. Meals processing and threat of inflammatory bowel illness: a scientific assessment and meta-analysis. Clin Gastroenterol Hepatol. 2023. doi: 10.1016/j.cgh.2023.01.012.
- Camilleri M, Vella A. What to do concerning the leaky intestine. Intestine. 2022; 71(2):424-435. doi: 10.1136/gutjnl-2021-325428.
Further references on intestine microbiota and IBD:
- Ramos, G. P., and Papadakis, Ok. A. (2019). Mechanisms of illness: inflammatory bowel illnesses. Mayo Clin. Proc. 94, 155–165.
- Ma, Y., Xu, X., Li, M., Cai, J., Wei, Q., and Niu, H. (2019). Intestine microbiota promote the inflammatory response within the pathogenesis of systemic lupus erythematosus. Mol. Med. 25:35.
- O’Donnell, S., Borowski, Ok., Espin-Garcia, O., Milgrom, R., Kabakchiev, B., Stempak, J., et al. (2019). The unsolved hyperlink of genetic markers and crohn’s illness development: a north american cohort expertise. Inflamm. Bowel Dis. 25, 1541–1549.
- Pang, J. X. Q., Kheirkhahrahimabadi, H., Bindra, S., Bindra, G., Panaccione, R., Eksteen, B., et al. (2021). Differential impact of genetic burden on illness phenotypes in Crohn’s illness and ulcerative colitis in a Canadian cohort. J. Can. Assoc. Gastroenterol. 4, 65–72.
- Zheng, D., Liwinski, T., and Elinav, E. (2020). Interplay between microbiota and immunity in well being and illness. Cell Res. 30, 492–506.
- Andoh, A., Kuzuoka, H., Tsujikawa, T., Nakamura, S., Hirai, F., Suzuki, Y., et al. (2012). Multicenter evaluation of fecal microbiota profiles in Japanese sufferers with Crohn’s illness. J. Gastroenterol. 47, 1298–1307.
- Joossens, M., Huys, G., Cnockaert, M., De Preter, V., Verbeke, Ok., Rutgeerts, P., et al. (2011). Dysbiosis of the faecal microbiota in sufferers with Crohn’s illness and their unaffected kin. Intestine 60, 631–637.
- Darfeuille-Michaud, A., Boudeau, J., Bulois, P., Neut, C., Glasser, A. L., Barnich, N., et al. (2004). Excessive prevalence of adherent-invasive Escherichia coli related to ileal mucosa in Crohn’s illness. Gastroenterology 127, 412–421.
- Liu, S., Zhao, W., Lan, P., and Mou, X. (2020). The microbiome in inflammatory bowel illnesses: from pathogenesis to remedy. Protein Cell 15, 331–345.
- Iliev, I. D., and Leonardi, I. (2017). Fungal dysbiosis: immunity and interactions at mucosal obstacles. Nat. Rev. Immunol. 17, 635–646.
- Beheshti-Maal, A., Shahrokh, S., Ansari, S., Mirsamadi, E. S., Yadegar, A., Mirjalali, H., et al. (2021). Intestine mycobiome: The possible determinative position of fungi in IBD sufferers. Mycoses 64, 468–476.
- Sokol, H., Leducq, V., Aschard, H., Pham, H. P., Jegou, S., Landman, C., et al. (2017). Fungal microbiota dysbiosis in IBD. Intestine 66, 1039–1048.
- Qiu, X., Ma, J., Jiao, C., Mao, X., Zhao, X., Lu, M., et al. (2017). Alterations within the mucosa-associated fungal microbiota in sufferers with ulcerative colitis. Oncotarget 8, 107577–107588.
- Inczefi, O.; Bacsur, P.; Resal, T.; Keresztes, C.; Molnar, T. The Affect of Vitamin on Intestinal Permeability and the Microbiome in Well being and Illness. Entrance. Nutr. 2022, 9, 718710.
- Lo Sasso, G.; Khachatryan, L.; Kondylis, A.; Battey, J.N.D.; Sierro, N.; Danilova, N.A.; Grigoryeva, T.V.; Markelova, M.I.; Khusnutdinova, D.R.; Laikov, A.V.; et al. Inflammatory Bowel Illness-Related Modifications within the Intestine: Give attention to Kazan Sufferers. Inflamm. Bowel Dis. 2021, 27, 418–433.
- Palumbo VD, Romeo M et al. (2016), The long-term results of probiotics within the remedy of ulcerative colitis: A scientific research. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub; 160(3):372-377.
- Rodolico V, Tomasello G et al. (2010), Hsp60 and Hsp10 enhance in colon mucosa of Crohn’s illness and ulcerative colitis. Cell Stress and Chaperones vol. 15, 877–884.
- Bellavia M, Tomasello G, Romeo M et al. (2013), Intestine microbiota imbalance and chaperoning system malfunction are central to ulcerative colitis pathogenesis and may be counteracted with particularly designed probiotics: a working speculation. Medical Microbiology and Immunology vol. 202, 393–406
- Tomasello G, Sciumé C et al. (2011), Hsp10, Hsp70, and Hsp90 immunohistochemical ranges change in ulcerative colitis after remedy. Eur J Histochem; 55(4):e38.
- Tomasello G, Palumbo VD et al. (2014), Probiotics and traditional terapy: new fronter in therapeutic strategy in articular manifestations of IBD. Progress in Vitamin 2014; Vol. 16 N. 3: 176-187